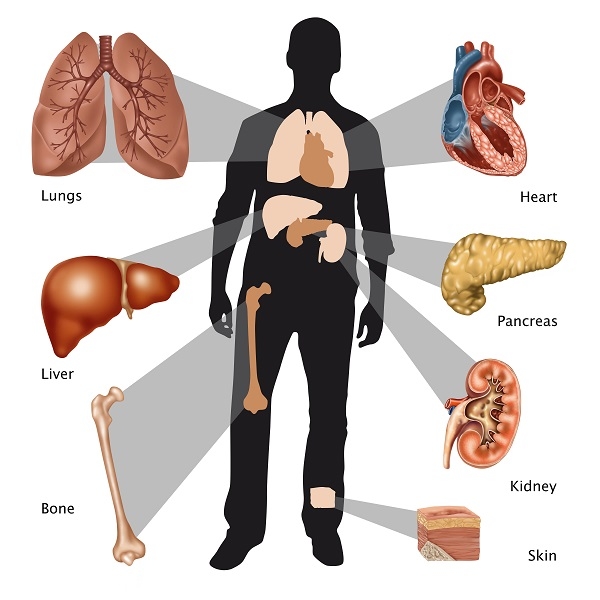
Organ transplantation is a life-saving medical procedure that replaces a failing organ with a healthy one from a donor. However, after transplantation, the recipient’s immune system may recognize the transplanted organ as foreign and mount an immune response, leading to rejection. Preventing rejection is crucial for the long-term success of organ transplantation. This blog explores the mechanisms of organ rejection, types of rejection, current preventive strategies, challenges in transplantation, and emerging research in the field. Azathioprine 50 Mg Tablet is used with other medicines to prevent your body from rejecting an organ (such as a kidney, heart, or liver) after a transplant.
Mechanisms of Organ Rejection:
Organ rejection occurs when the recipient’s immune system identifies the transplanted organ as foreign and attacks it. The immune response involves several key steps:
-
Recognition Phase:
- Antigen Presentation: Immune cells (such as dendritic cells) present donor antigens (proteins) from the transplanted organ to T-cells, triggering an immune response. Azoran 50 Tablet belongs to a group of medicines called immunosuppressants.
- T-Cell Activation: T-cells become activated and produce cytokines that promote inflammation and recruit more immune cells to the site of the transplanted organ.
-
Effector Phase:
- Cellular Rejection (Acute Rejection): Involves direct attack on donor cells by activated T-cells, leading to tissue damage.
- Humoral Rejection (Antibody-Mediated Rejection): Antibodies produced against donor antigens bind to the transplanted organ’s cells, leading to complement activation and tissue injury.
Types of Rejection:
-
Acute Rejection:
- Typically occurs within the first few months after transplantation.
- Characterized by T-cell-mediated immune response against the donor organ.
- Can be asymptomatic or present with fever, swelling, pain, or dysfunction of the transplanted organ.
-
Chronic Rejection:
- Develops gradually over months to years.
- Involves ongoing immune-mediated damage to the transplanted organ’s blood vessels and tissues.
- Results in progressive fibrosis and organ dysfunction.
Strategies to Prevent Organ Rejection:
Effective prevention of organ rejection involves a combination of immunosuppressive medications, monitoring for rejection signs, and patient management strategies:
-
Immunosuppressive Medications:
-
Calcineurin Inhibitors (CNI): Examples include tacrolimus and cyclosporine. These drugs prevent T-cell activation and cytokine production.
-
Antiproliferative Agents: Drugs like mycophenolate mofetil (MMF) inhibit T-cell and B-cell proliferation.
-
Corticosteroids: Reduce inflammation and suppress immune responses.
-
Biological Agents: Monoclonal antibodies (e.g., basiliximab, alemtuzumab) target specific immune cells or cytokines involved in rejection.
-
-
Induction Therapy:
- Intensive immunosuppression immediately after transplantation to prevent acute rejection.
- Often includes high-dose corticosteroids and potent immunosuppressants.
-
Maintenance Therapy:
- Long-term use of immunosuppressive medications to prevent both acute and chronic rejection.
- Adjusted based on patient response, drug levels, and risk of side effects.
-
Monitoring and Surveillance:
- Regular monitoring of immunosuppressant drug levels (therapeutic drug monitoring) to ensure adequate suppression of immune responses while minimizing side effects.
- Biopsies and imaging studies (e.g., ultrasound, Doppler) to assess organ function and detect signs of rejection early.
-
Patient Education and Compliance:
- Educating patients about the importance of adhering to medication schedules, monitoring for signs of rejection, and managing potential side effects.
- Encouraging lifestyle modifications (e.g., smoking cessation, healthy diet) to optimize transplant outcomes.
Challenges in Organ Transplantation:
Despite advances in immunosuppressive therapies, challenges in organ transplantation persist:
-
Rejection Risk: Some patients may experience acute or chronic rejection despite optimal immunosuppression.
-
Side Effects: Long-term use of immunosuppressive drugs can increase the risk of infections, cardiovascular disease, diabetes, and kidney dysfunction.
-
Organ Shortage: Limited availability of donor organs remains a significant barrier to transplantation for many patients.
-
Cost and Accessibility: Access to transplantation and post-transplant care may be limited by financial barriers or geographic disparities.
Emerging Research and Future Directions:
Researchers are exploring new approaches to improve outcomes in organ transplantation:
-
Immune Tolerance Induction:
- Developing strategies to induce immune tolerance, allowing transplant recipients to accept donor organs without long-term immunosuppression.
-
Biological Therapies:
- Investigating novel biological agents and monoclonal antibodies to target specific immune pathways involved in rejection.
-
Gene Editing and Cell Therapy:
- Using gene editing technologies (e.g., CRISPR/Cas9) to modify immune cells or donor organs to reduce rejection risk.
-
Organ Preservation Techniques:
- Enhancing methods for organ preservation and transportation to improve transplant outcomes.
Conclusion:
Preventing rejection of transplanted organs is essential for the success and longevity of organ transplantation. By understanding the mechanisms of rejection, utilizing effective immunosuppressive medications, monitoring for signs of rejection, and addressing challenges in transplantation, healthcare providers can optimize patient outcomes. Ongoing research into immune tolerance, biological therapies, and organ preservation techniques holds promise for further improving transplant outcomes and quality of life for transplant recipients. Continued collaboration between clinicians, researchers, and patients is crucial in advancing the field of organ transplantation and addressing the complexities of immune responses and rejection. For individuals undergoing transplantation, early detection of rejection signs and adherence to treatment plans are vital for achieving long-term graft survival and improved quality of life.